What’s next?
When we had our first meeting with the neurosurgeon, we were unsure what to expect. We were hoping for some kind of plan for what to do next but, by the end of the meeting, we knew even less than we did at the start.
Our surgeon said:
You should expect very little certainty on this journey.
Since then, we have had a bunch of MRIs that each seemed to say different things. The tumour was in three lobes (temporal, frontal & insula) or it was in two lobes (temporal & parietal). It infiltrated half a hemisphere or it filled my temporal lobe entirely.
We had no idea what subtype or grade the tumour is and we can’t even begin treatment without that information. We decided to have a biopsy to eliminate some uncertainty (I gots to know). One four-inch scar and a titanium plate later, we waited for the results. Eleven long weeks went by until we met with our medical team to hear the score.
And the results were…
** drumroll **
The results were inconclusive.
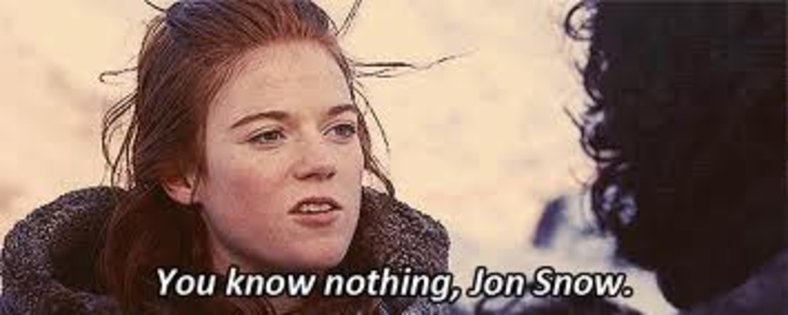
Three different pathologists gave three different reports that ranged from “dunno” to “probably a glioma” to “might be an astrocytoma”. The molecular profiling found nothing interesting at all. We are back where we started: We know nothing.
The docs gave us three options:
1. I can have a craniotomy to get a better biopsy. Apparently, most people don’t really use their anterior temporal lobe so he can take a chunk of that.
The anterior temporal lobe (ATL) is thought to be critical for semantic memory–our knowledge of objects, people, words, and facts.
The Journal of Neuroscience
2. There are two possible chemo treatments, PCV & TMZ. Which one you choose depends on the subtype and grade. Since we don’t know either, we could flip a coin and cross our fingers that we chose the right one.
Procarbazine, lomustine (also known as CCNU) and vincristine is a combination of chemotherapy drugs.
Cancer Research UK
Temozolomide (TMZ) is a chemotherapy drug that has been shown to improve average survival rate for people with some high grade brain tumours.
The Brain Tumour Charity
3. We could do nothing and decline treatment entirely.
We chose door number 3.
We’ll get an MRI every six months to see if the tumour has grown and, meanwhile, we’ll just get on with our lives and forget all about brain tumours until the next scan.

